if diagnosed at Stage I
if diagnosed at Stage II
if diagnosed at Stage III
if diagnosed at Stage IV

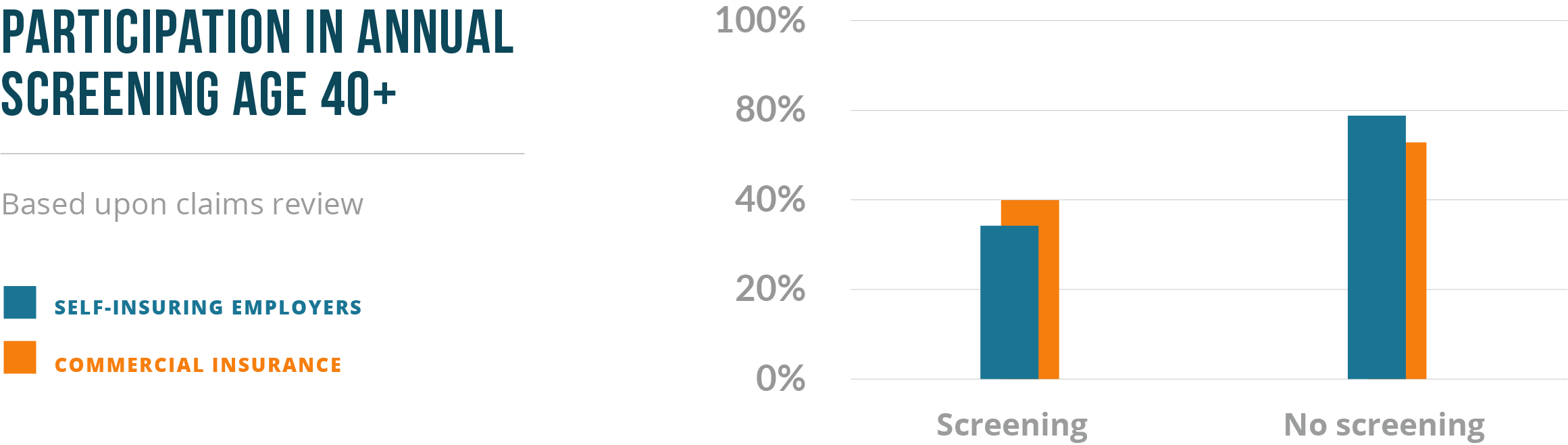
When we work with an employer, health plan, TPA, or insurer and we examine claims history to see how many women age 40 and above have annual mammograms, the most common answer is 25% to 40%; at those adoption levels, commonly half or more breast cancers are detected at late stages. When we look back at adoption over time, adoption of mammograms has been declining for years. Adoption is always lower in minority populations and of course there’s no early detection solution for AfricanAmerican women age 35 to 39.
Without effective and widely adopted early detection, the proportion of cancers not detected until a late stage increases dramatically and cancer care costs increase greatly.
Many women and in fact many physicians have “heard,” that women shouldn’t have mammograms until age 50 and even then, not more than every other year.
Tragically, this is often confused as a declaration that there’s no need for annual early detection for women 40-49 - but their risk hasn’t changed. In fact cancer frequency is increasing in women 40-45. This suggestion of “only after age 50,” aims to limit the use of mammograms as a screening technology, primarily because they produce too many falsely positive results.
Annual early detection beginning at age 40 remains the guideline that most reduces suffering and death - all medical groups with expertise in breast cancer care support annual early detection beginning at age 40. Women who will not our cannot have a mammogram shouldn’t be left behind in the face of the most common women’s cancer. They need another option.